Providing access to healing, well-being and empowerment
A program by the Patcha Foundation and Immigrant Community Services


We support you with services, education, and resources.




HIV Testing & More.


Why HIVE?
You don’t have to do this alone
We most commonly know the term hive from Bee Hives. Bee Hives are essential to supporting colonies, bee networks, communication, and the creation of honey. Honey development leads to a healthy food source that supports nutrients and healing well beyond its community. The Hive is our model for creating a network for providing access to healing, well-being and empowerment.
We want you to join our Hive. We are a support organization that provides services, education, and lifestyle resources. We are all the buzz about town, serving the Metro Maryland community. To ensure you have the support you need, we will connect you to the right services and resources for appointments, to guide you through networks and help answer questions that may be intimidating, confusing or simply frustrating.


The HIVE (HIV Engagement) program was established in 2021 by the Patcha Foundation (patchafoundation.org) and Immigrant Community Services (immiserve.org) to support targeted outreach to racial and ethnic minority persons with HIV in Montgomery County, Maryland and Prince George’s County, Maryland who are not engaged in HIV medical care and provide linkage to HIV medical care, medication assistance programs, and other needed health and support services. These services were provided as part of the Ryan White HIV/AIDS Program Part B Minority AIDS Initiative (MAI) program which seeks to improve access to HIV care and health outcomes for disproportionately affected racial/ethnic minority populations and increase racial/ethnic minority participation in the Maryland AIDS Drug Assistance Program (MADAP) and other medication assistance programs.
More than half of people with diagnosed HIV in the United States receive services through the Ryan White HIV/AIDS Program each year. That means more than half a million people received services through the program. For more follow this link https://hab.hrsa.gov/about-ryan-white-hivaids-program.
MAI was established in 1999 by Congress under the Ryan White HIV/AIDS Program Parts A, B, C, and D to improve access to HIV care and health outcomes for disproportionately affected minority populations, including black populations. Link to more https://hab.hrsa.gov/about-ryan-white-hivaids-program/part-f-minority-aids-initiative


Need Help? Call Us Now: (301) 850 2991
We can help you get the appropriate consultation and resources you may need.
What is HIV?
HIV (human immunodeficiency virus) is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases. The human body can’t get rid of HIV and no effective HIV cure exists. So, once you have HIV, you have it for life. However, by taking HIV medicine (called antiretroviral therapy or ART), people with HIV can live long and healthy lives and prevent transmitting HIV to their sexual partners. In addition, there are effective methods to prevent getting HIV through sex or drug use, including pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
“The only way to know if you have HIV is to get tested”
How Is HIV Transmitted?
You can only get HIV by coming into direct contact with certain body fluids from a person with HIV who has a detectable viral load. These fluids are: Blood, Semen (cum) and pre-seminal fluid, Rectal fluids, Vaginal fluids, Breast milk.
For transmission to occur, the HIV in these fluids must get into the bloodstream of an HIV-negative person through a mucous membrane (found in the rectum, vagina, mouth, or tip of the penis); open cuts or sores; or by direct injection.
Ways HIV cannot be Transmitted:
HIV is not spread by: Air or water, Mosquitoes, ticks or other insects, Saliva, tears, or sweat that is not mixed with the blood of a person with HIV, Touching Unbroken skin of another person. i.e. Shaking hands, hugging, Drinking fountains, Other sexual activities that don’t involve the exchange of body fluids (for example, touching).
How HIV Viral Load Affects Transmitting HIV?
Viral load is the amount of HIV in the blood of someone who has HIV. Taking HIV medicine (called antiretroviral therapy or ART) daily as prescribed can make the viral load very low—so low that a test can’t detect it (this is called an undetectable viral load).
People with HIV who take HIV medicine daily as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to an HIV-negative partner through sex.
HIV medicine is a powerful tool for preventing sexual transmission of HIV. But it works only as long as the HIV-positive partner gets and keeps an undetectable viral load. Not everyone taking HIV medicine has an undetectable viral load. To stay undetectable, people with HIV must take HIV medicine every day as prescribed and visit their healthcare provider regularly to get a viral load test.

What We Do
The AIDS Drug Assistance Program (MADAP) provides HIV-related prescription drugs to underinsured and uninsured individuals living with HIV/AIDS and can help pay insurance premiums. Our team can help you to figure out if you qualify for MADAP. You don’t need an appointment to see our team. Team members are available to assist you.
The Patcha Foundation is committed to improving the health and well-being of marginalized communities through federal and local advocacy, education, and research. The HIVE welcomes and highlights support for Indigenous African communities, African-Americans and the LGBTQ community, including individuals of every sexual orientation, and age regardless of disability, income, education, and geography.
Our team is here to talk with you about your health insurance options and any problems you are having with insurance or the cost of your care. We will meet with any HIVE client who doesn’t have insurance to see what they qualify for and to help them enroll. Our goal is to help you find an insurance plan that meets your needs and help you navigate any insurance issues.
Slowing the Spread
Since there is no HIV vaccine it is important to take every measure to prevent it from spreading.
Use treatment as prevention (TasP): If you’re living with HIV, taking HIV medication can keep your partner from becoming infected with the virus. If you make sure your viral load stays undetectable — a blood test doesn’t show any virus — you won’t transmit the virus to anyone else. Using TasP means taking your medication exactly as prescribed and getting regular checkups.
Use post-exposure prophylaxis (PEP) if you’ve been exposed to HIV:
If you think you’ve been exposed through sex, needles or in the workplace, contact your doctor or go to the emergency department. Taking PEP as soon as possible within the first 72 hours can greatly reduce your risk of becoming infected with HIV. You will need to take medication for 28 days.
Use a new condom every time you have sex: Use a new condom every time you have anal or vaginal sex. Women can use a female condom. If using a lubricant, make sure it’s water-based. Oil-based lubricants can weaken condoms and cause them to break. During oral sex use a nonlubricated, cut-open condom or a dental dam — a piece of medical-grade latex.
Consider preexposure prophylaxis (PrEP): The combination drugs emtricitabine plus tenofovir (Truvada) and emtricitabine plus tenofovir alafenamide (Descovy) can reduce the risk of sexually transmitted HIV infection in people at very high risk. PrEP can reduce your risk of getting HIV from sex by more than 90% and from injection drug use by more than 70%, according to the Centers for Disease Control and Prevention. Descovy hasn’t been studied in people who have receptive vaginal sex.
Your doctor will prescribe these drugs for HIV prevention only if you don’t already have HIV infection: You will need an HIV test before you start taking PrEP and then every three months as long as you’re taking it. Your doctor will also test your kidney function before prescribing Truvada and continue to test it every six months.
You need to take the drugs every day: They don’t prevent other STIs, so you’ll still need to practice safe sex. If you have hepatitis B, you should be evaluated by an infectious disease or liver specialist before beginning therapy.
Tell your sexual partners if you have HIV: It’s important to tell all your current and past sexual partners that you’re HIV-positive. They’ll need to be tested.
Use a clean needle: If you use a needle to inject drugs, make sure it’s sterile and don’t share it. Take advantage of needle-exchange programs in your community. Consider seeking help for your drug use.

A Healthy Body & Preventing Infections
There are various antiretroviral drugs, so let’s discuss how they work, and their possible side effects.
Antiretroviral Therapy (ART)
Antiretroviral therapy reduces the amount of HIV in the body. When a person takes them consistently, antiretroviral drugs are very effective at limiting the impact of the virus. This therapy helps keep the body healthy and prevent infections. Specifically, successful antiretroviral therapy prevents people from developing advanced HIV and makes it impossible to transmit the virus to others. The Centers for Disease Control and Protection (CDC) recommends that all people with HIV take antiretroviral therapy, regardless of how long they have had the virus or their current state of health.
Antiretroviral therapy has become more potent, less toxic, and easier to use than in the past. It produces fewer and less severe side effects than before.
Trouble sleeping? These side effects can be caused by different types of ART medication, so it is important to check with your doctor which specific medication you should be taking. If you need help finding the right type of medication for you, contact us so we can connect you to the right help.
How does antiretroviral treatment work?
ART stops HIV from making copies of itself. This keeps the amount of virus in your body low, protecting your immune system so you’re less likely to get sick. With good healthcare and treatment, people with HIV can expect to live as long as people who don’t have HIV. You can continue to have relationships, to work or study, to make plans, to have a family – whatever you would have done before your HIV diagnosis.
By keeping the amount of HIV in your body low, ART also reduces the risk of HIV being passed on. People living with HIV who take their treatment properly (at the right times and as advised by a doctor) can achieve something called an ‘undetectable viral load’. This is when the amount of HIV in their body has been reduced to such low levels that it can’t be passed on through sex. To know if you have an undetectable viral load, it’s important to attend regular appointments with your healthcare team to have your viral load measured – this can tell you how effective your treatment is and how much HIV there is in your body.
Some Side effects of ART are: Appetite loss, Diarrhea, Fatigue, Higher than normal levels of cholesterol and triglycerides, Mood changes, depression, and anxiety, Nausea and vomiting, and Rash.
Creating a Treatment Schedule
If you need help establishing a routine or plan here are some tips that may help you take every dose of your HIV medication, every day.
Getting Started
Follow The Treatment
Create a Routine
Get Good Support
When starting their HIV treatment many people are hesitant to take the medication because they fear a loss of autonomy. These fears of being “locked into a strict routine of medicine-taking,” makes many feel like they have no independence over their life. This is an aspect of a chronic illness like HIV that many don’t consider how much it changes a person’s life. But what many also don’t realize when taking HIV medication is that they don’t work for the medication. The medication works for you. Just by deciding to take the medicine you are making a decision to fight HIV and preventing it from controlling your life. Taking your medication can be as easy as brushing your teeth in the morning. You just need the right plan.
Follow your treatment plan exactly as your healthcare provider has prescribed. HIV medication should be taken at specific times of the day, with or without certain kinds of food. If you have questions about when and how to take your medication, talk to your health care provider or pharmacist.
Create a routine. Add taking your medication to things you already do each day. For example, if your medical provider prescribes taking your medication every morning with food, make it a habit to take it at breakfast. Try a weekly or monthly pill box with compartments for each day of the week to help you remember whether or not you took your medicine that day. Set an alarm on your clock, watch, or phone for the time you take your HIV medication. Keep a daily log or use a calendar to keep track of the days you have taken your HIV medication.
Download a free app from the Internet to your computer or on your smartphone that can help remind you when it’s time to take your HIV medication. Search for “reminder apps,” and you will find many choices. Set up automatic refills at your pharmacy. Your medicine will be ready when you need it, and you won’t run out.
Ask a family member or friend to encourage you and give you a daily phone call, text, or email to remind you to take your HIV medication. Continue to see your health care provider regularly. Regular medical visits are important to monitor the amount of virus in your blood to make sure it stays undetectable, and to receive other medical support. Use these visits to talk openly to your provider about any help you might need sticking to your treatment plan.
Contact us if you need help getting connected to HIV resources or have a question.
When starting their HIV treatment many people are hesitant to take the medication because they fear a loss of autonomy. These fears of being “locked into a strict routine of medicine-taking,” makes many feel like they have no independence over their life. This is an aspect of a chronic illness like HIV that many don’t consider how much it changes a person’s life. But what many also don’t realize when taking HIV medication is that they don’t work for the medication. The medication works for you. Just by deciding to take the medicine you are making a decision to fight HIV and preventing it from controlling your life. Taking your medication can be as easy as brushing your teeth in the morning. You just need the right plan.
Follow your treatment plan exactly as your healthcare provider has prescribed. HIV medication should be taken at specific times of the day, with or without certain kinds of food. If you have questions about when and how to take your medication, talk to your health care provider or pharmacist.
Create a routine. Add taking your medication to things you already do each day. For example, if your medical provider prescribes taking your medication every morning with food, make it a habit to take it at breakfast. Try a weekly or monthly pill box with compartments for each day of the week to help you remember whether or not you took your medicine that day. Set an alarm on your clock, watch, or phone for the time you take your HIV medication. Keep a daily log or use a calendar to keep track of the days you have taken your HIV medication.
Download a free app from the Internet to your computer or on your smartphone that can help remind you when it’s time to take your HIV medication. Search for “reminder apps,” and you will find many choices. Set up automatic refills at your pharmacy. Your medicine will be ready when you need it, and you won’t run out.
Ask a family member or friend to encourage you and give you a daily phone call, text, or email to remind you to take your HIV medication. Continue to see your health care provider regularly. Regular medical visits are important to monitor the amount of virus in your blood to make sure it stays undetectable, and to receive other medical support. Use these visits to talk openly to your provider about any help you might need sticking to your treatment plan.
Contact us if you need help getting connected to HIV resources or have a question.
Links to help you
Contact us today to see how you can volunteer with us.
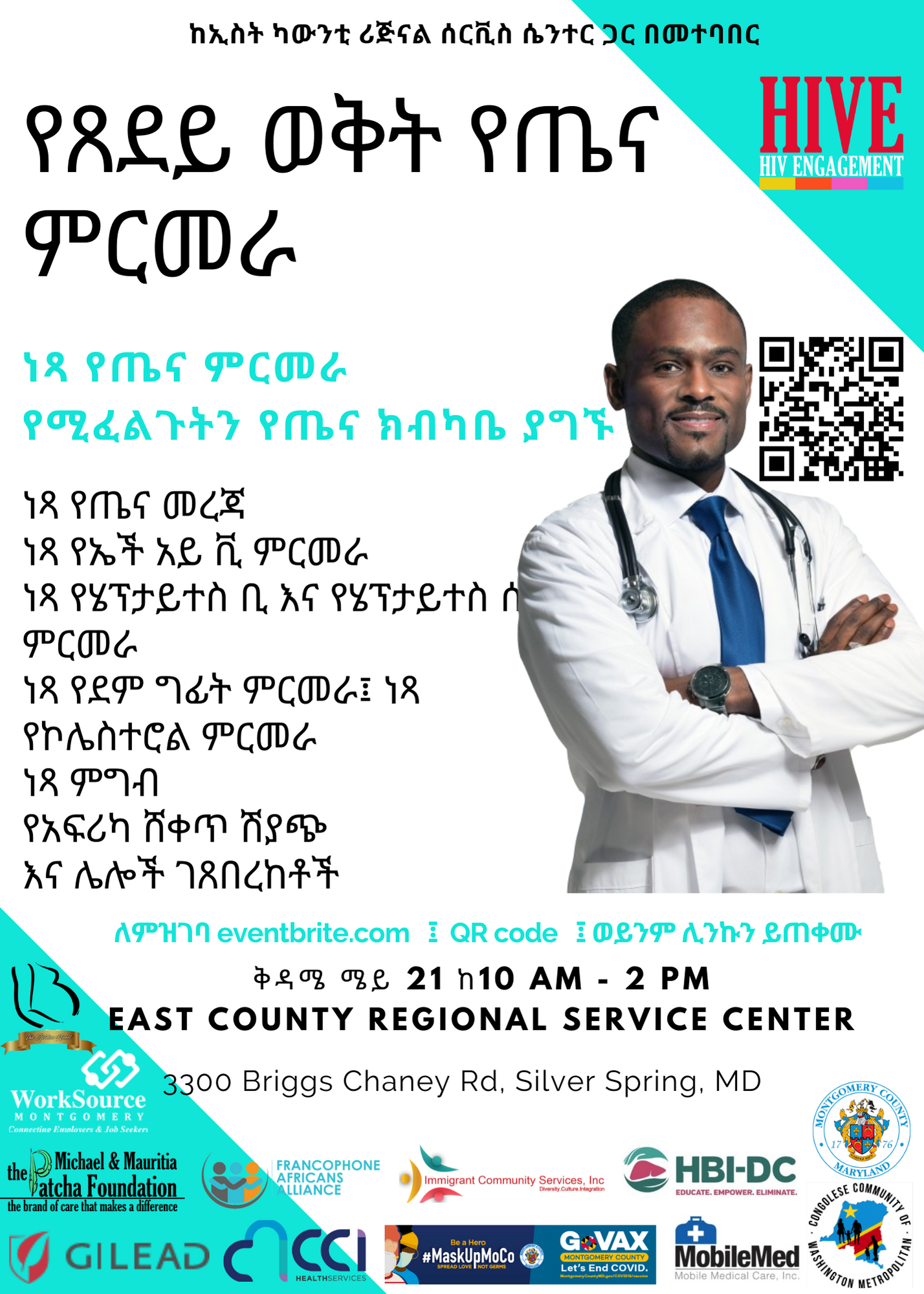
2022 Spring Health Fair
Community Event
2022 Spring Health Fair
This event will be held at the East County Regional Service Center, in the 20904-zip code area which has been identified by Maryland Department of Health as one of the red zones with a high population of people living with HIV. The event will be free for those who attend, and we will provide free medical resources, information, and health screenings such as Hepatitis B & C, cholesterol, blood pressure checks, COVID Vaccines and HIV testing.
REGISTER HERE
or scan the QR code in the flyers
Weekly Support Group
Weekly Support Group
Join us for weekly meetings and discussions about living with the challenges of HIV and AIDS.
The group focuses on supporting individuals by providing a safe space to share experiences, information on available resources, promoting sense of community for Positive Healthy Living.
REGISTER HERE
Call us at: 240-277-1310

Register for HIVE Tranquility Lounge
Please complete our quick registration form in order to secure your spot for testing.Featured News and Events
Get in Touch
We specifically serve Prince Georges & Montgomery County, Maryland.